Background: High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements (HGBL-DH/TH) is a recently defined category in the latest revision of the World Health Organization (WHO) classification, which comprises approximately 5-15% of newly diagnosed DLBCL. This subtype of lymphoma poses numerous challenges from diagnosis to treatment of patients. On the one hand, diagnosis of HGBL-DH/TH requires the accomplishment of fluorescent in-situ hybridization (FISH) to identify the translocations of MYC(8q24) and BCL2(18q21) or/and BCL6(3q27), with no consensus being reached regarding the most applicable population for FISH tests due to high cost and low prevalence. On the other hand, HGBL-DH/TH displays aggressive features, including a high incidence of advanced disease at diagnosis, and inferior efficacy to standard-induced chemical immunotherapy with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). Despite several treatment strategies including intensified protocols and hematopoietic cell transplantation (HCT) have been explored, there is no standard regimen to improve outcomes for HGBL patients, and participation in clinical trials is encouraged.
Aims: This study aims to investigate the clinical characteristics and prognostic outcomes of HGBL-DH/TH patients, and performed genomic and transcriptomic analyses to link the oncogenic mutations and tumor microenvironment alterations to different DLBCL subgroups.
Method:In this study, 107 patients with newly diagnosed HGBL-DH/TH were analyzed. Histological diagnoses were established according to the WHO classification. These HGBL-DH/THs were termed DHL-BCL2 (MYC and BCL2 translocation), DHL-BCL6 (MYC and BCL6 translocation), and THL in our study. DNA sequencing was carried out on 95 patients, for detection of genetic aberrations.
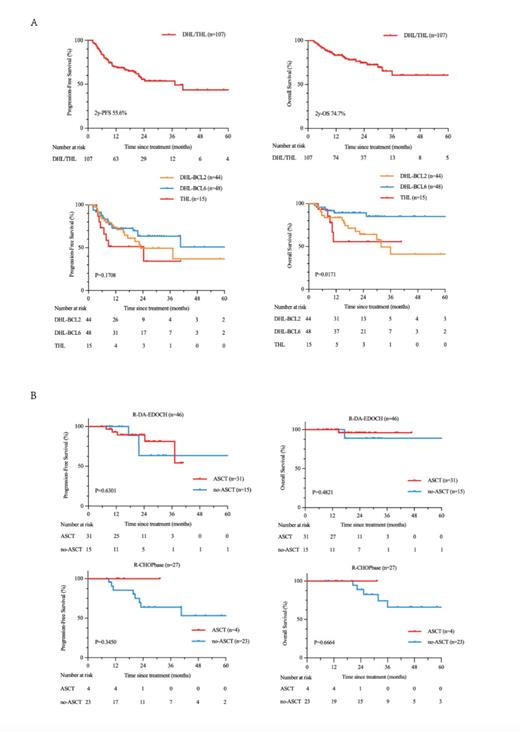
Results: Patients with DHL-BCL2 (n=44) and THL (n=15) have similar clinical features, including elevated serum lactate dehydrogenase (LDH), increased proportion of double expression (DE) as well as increased prevalence of non-GCB subtype compared to those with DHL-BCL6 (n=48). With the median follow-up time of 19.3 months (2.5-114.2 months), patients in the DHL-BCL2 and THL group had dismal survival (2-year PFS: 49.3% and 34.2%; 2-year OS: 64.0% and 55.6%) when compared with those in the DHL-BCL6 group (2-year PFS: 63.5%; 2-year OS: 89.3%) (Figure A). Moreover, intensive chemoimmunotherapy or combination with novel targeted agents seemed to improve outcomes in patients with DHL/THL compared with those who received a standard R-CHOP regime. The use of autologous stem cell transplant (ASCT) did not yield a significant improvement in survival for patients who achieved remission after receiving first-line R-DA-EDOCH therapy. However, it is worth noting that there was a trend towards prolonging progression-free survival (PFS) and overall survival (OS) in patients who achieve complete remission (CR) through RCHOP-based treatment and undergo ASCT (Figure B). Compared to DHL-BCL6, the primary genetic lesions in DHL-BCL2 and THL were alterations associating epigenetic regulators like EZH2 and CREBBP, while the primary genetic lesions in DHL-BCL6 were alterations associating cellular differentiation and transcription factors like BTG2, PTPN6, CD70, and BCL6. Correlatively, the EZB genotype was more frequently observed in patients with DHL-BCL2 and THL, while the BN2 genotype was more frequently observed in patients with DHL-BCL6.
Conclusion: DHL-BCL2/THL exhibits similar clinical characteristics, prognostic outcomes, and molecular features that set it apart from DHL-BCL6. This implies the need for testing novel agents or therapeutic strategies to expedite treatment development for patients with DHL-BCL2/THL.
Disclosures
No relevant conflicts of interest to declare.